COPD or Chronic obstructive pulmonary disease is slowly progressive obstruction of airflow into or out of the lungs.
Thank you for reading this post, don't forget to subscribe!The incidence of COPD has almost doubled since 1982. The symptoms (for example, shortness of breath, coughing) come on slowly and many people are consequently diagnosed after age 40-50, although some are diagnosed at a younger age. COPD patients may exhibit symptoms of chronic, bronchitis, emphysema and asthma.
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) defines chronic obstructive pulmonary disease as airflow limitation that is not fully reversible, usually progressive and is associated with an abnormal inflammatory response of the lungs to inhaled noxious particles or gases. This information will focus on chronic obstructive pulmonary disease and not on other related problems (for example, chronic bronchitis or asthma).
The cause of COPD is usually long-term exposure to irritants that damage lungs and airways. The life expectancy for individuals with chronic obstructive pulmonary disease (COPD) ranges from good to poor, depending on the person’s COPD stage and of course treatment method, with a decreasing outlook as the disease progresses toward stage IV (end-stage) chronic obstructive pulmonary disease.
Five Common symptoms of the chronic obstructive pulmonary disease
-
- cough,
- chest discomfort,
- shortness of breath,
- wheezing, and
- fatigue.
- Progressive or more serious symptoms may include
- respiratory distress,
- tachypnea,
- cyanosis,
- use of accessory respiratory muscles,
- peripheral edema,
- hyperinflation,
- chronic wheezing,
- abnormal lung sounds,
- prolonged expiration,
- elevated jugular venous pulse, and
- cyanosis.
Symptoms
Chronic obstructive pulmonary disease is a slowly progressive disease so it is not unusual for the initial signs and symptoms to be a bit different from those in the late stages of the disease.
There are many ways to evaluate or stage chronic obstructive pulmonary disease, often based on symptoms. Usually, the first signs and symptoms of COPD include a productive cough usually in the morning, with colorless or white mucus (sputum).
The most significant symptom of chronic obstructive pulmonary disease is breathlessness, termed shortness of breath (dyspnea). Early on, this symptom may occur occasionally with exertion and eventually may progress to breathlessness while doing a simple task such as standing up or walking to the bathroom. Some people may develop wheezing (a whistling or hissing sound while breathing).
Five common signs and symptoms of the chronic obstructive pulmonary disease include:
- Cough, with usually colorless sputum in small amounts
- Acute chest discomfort
- Shortness of breath (usually occurs in patients aged 60 and over)
- Wheezing (especially during exertion)
- Fatigue
As the disease progresses from mild to moderate, symptoms often increase in severity:
- Respiratory distress with simple activities like walking up a few stairs
- Rapid breathing (tachypnea)
- Bluish discoloration of the skin (cyanosis)
- Use of accessory respiratory muscles
- Swelling of extremities (peripheral edema)
- Over-inflated lungs (hyperinflation)
- Wheezing with minimal exertion
- Course crackles (lung sounds usually with inspiration)
- Prolonged exhalations (expiration)
- Diffuse breath sounds
- Elevated jugular venous pulse.
Stages of chronic obstructive pulmonary disease COPD
One way to stage chronic obstructive pulmonary disease is the Global Initiative for Chronic Obstructive Lung Disease program (GOLD). The staging is based on the results of a pulmonary function test. Specifically, the forced expiratory volume (how much air one can exhale forcibly) in one second (FEV1) of a standard predicted value is measured, based on the individual patient’s physical parameters. The staging of chronic obstructive pulmonary disease by this method is as follows:
- Stage I is FEV1 equal to or more than 80% of the predicted value
- Stage II is FEV1 of 50% to 79% of the predicted value
- Stage III is FEV1 of 30% to 49% of the predicted value
- Stage IV is FEV1 of less than 30% of predicted value or an FEV1 less than 50% of predicted value plus respiratory failure.
Other staging methods are similar but are based on the severity of the shortness of breath symptom which is sometimes subjective. The above staging is measurable objectively, providing the patient is putting forth their best effort.
Causes of chronic obstructive pulmonary disease COPD?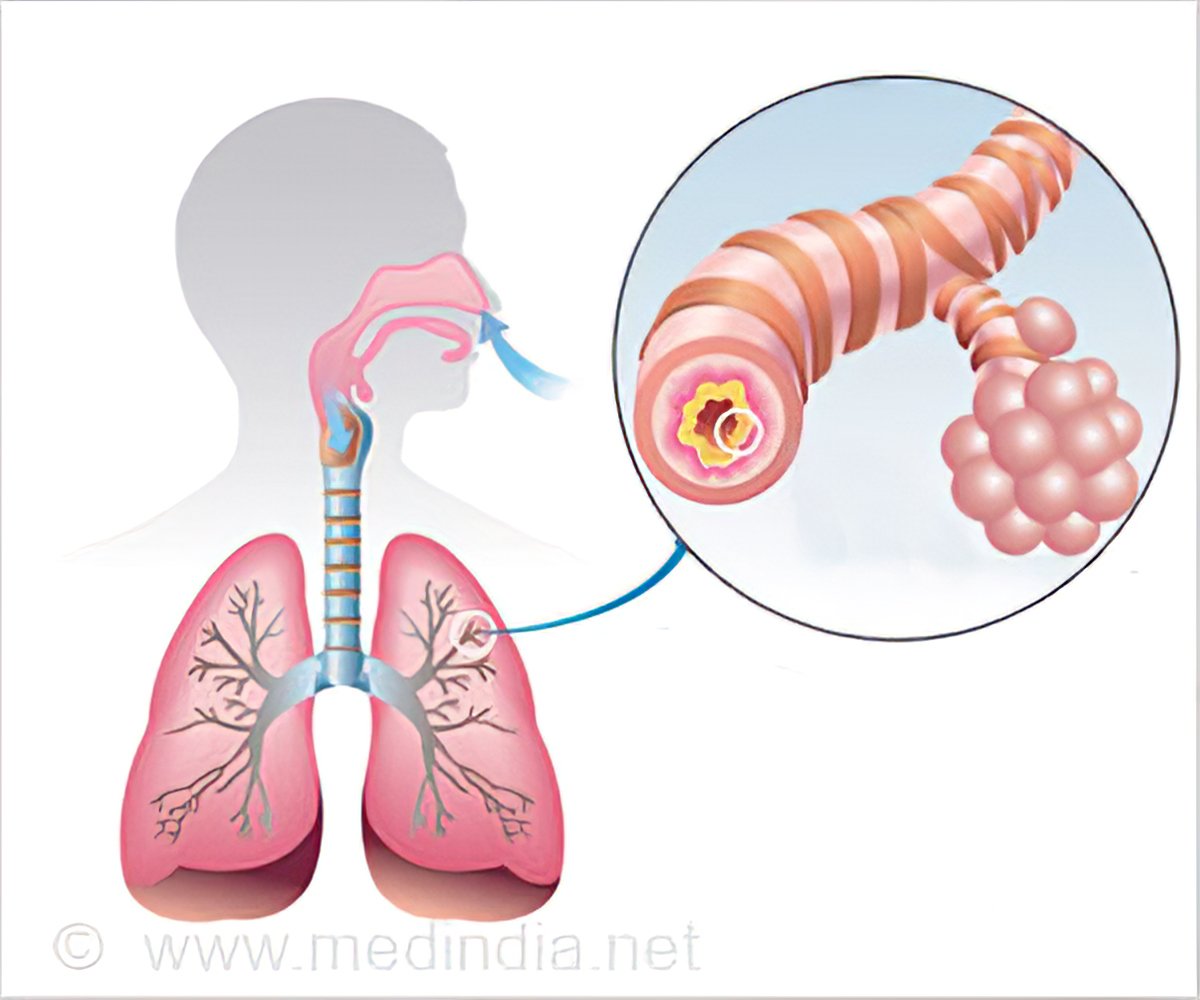
The primary cause of the chronic obstructive pulmonary disease is tobacco smoking or exposure to tobacco smoke. It is estimated that 90% of the risk for the development of chronic obstructive pulmonary disease is related to tobacco smoke. The smoke also can be secondhand smoke (tobacco smoke exhaled by a smoker and then breathed in by a non-smoker).
Other causes of chronic obstructive pulmonary disease are:
- Prolonged exposure to air pollution (burning coal, wood, chemicals, paints/colors, cement, mines, drug factories, textile etc).
- Infectious diseases: Infectious diseases that destroy lung tissue in patients with hyperactive airways or asthma also may contribute to causing this COPD.
Damage to the lung tissue over time causes physical changes in the tissues of the lungs and clogging of the airways with thick mucus. The tissue damage in the lungs leads to poor compliance (the elasticity, or ability of the lung tissue to expand). The decrease in elasticity of the lungs means that oxygen in the air cannot get by obstructions (for example, thick mucus plugs) to reach air spaces (alveoli) where oxygen and carbon dioxide exchange occurs in the lung. Consequently, the person exhibits a progressive difficulty, first coughing to remove obstructions like mucus, and then breathing, especially with exertion.
Risk factors for developing COPD
People who smoke tobacco are at the highest risk of developing chronic obstructive pulmonary disease. Other risk factors include exposure to secondhand smoke from tobacco and exposure to high levels of air pollution, especially air pollution associated with wood or coal. In addition, individuals with airway hyper-responsiveness such as those with chronic asthma are at increased risk.
There is a genetic factor called alpha-1 antitrypsin deficiency that places a small percentage (less than 1%) of people at higher risk for COPD (and emphysema) because of a protective factor (alpha-1 antitrypsin protein) for lung tissue elasticity is decreased or absent.
Other factors that may increase the risk of developing the chronic obstructive pulmonary disease include
- intravenous drug use,
- immune deficiency syndromes,
- vasculitis syndrome,
- connective tissue disorders, and
- genetic problems such as Salla disease (an autosomal recessive disorder of sialic acid storage in the body).
What other diseases or conditions contribute to COPD?
In general, three other non-genetic problems related to lung tissue play a role in chronic obstructive pulmonary disease. 1) chronic bronchitis, 2) emphysema, and 3) infectious diseases of the lung.
- Chronic bronchitis and emphysema, are thought by many to be variations of chronic obstructive pulmonary disease and are considered part of the progression of chronic obstructive pulmonary disease by many researchers. Chronic bronchitis is defined as a chronic cough that produces sputum for three or more months during two consecutive years.
- Emphysema is an abnormal and permanent enlargement of the air spaces (alveoli) located at the end of the terminal bronchioles in the lungs.
- Infectious diseases of the lung may damage areas of the lung tissue and contribute to chronic obstructive pulmonary disease.
Diagnosis of chronic obstructive pulmonary disease COPD
Doctors make a preliminary diagnosis of COPD in a person with chronic obstructive pulmonary disease symptoms by noting
symptoms by noting
- Patient’s breathing history,
- the history of tobacco smoking or exposure to secondhand smoke, and/or
- exposure to air pollutants, and/or a history of lung disease (for example, pneumonia, tuberculosis, asthma etc.).
Other tests to diagnose COPD
Other tests to diagnose COPD include:
- Chest X-rays
- CT scan of the lungs
- Arterial blood gas or a pulse oximeter to look at the saturation level of oxygen in the patient’s blood
Allopathic treatment for chronic obstructive pulmonary disease COPD
In allopathic treatment the first and best is to stop smoking immediately.
The treatments are often based on the stage of chronic obstructive pulmonary disease, for example:
- Stage I – short-acting bronchodilator as needed
- Stage II – short-acting bronchodilator as needed and long-acting bronchodilators plus cardiopulmonary rehabilitation
Medical treatments of chronic obstructive pulmonary disease drugs, for example, nicotine replacement therapy, beta-2 agonists and anticholinergic agents (bronchodilators), combined drugs using steroids and long-acting bronchodilators, mucolytic agents, oxygen therapy, and surgical procedures such as bullectomy, lung volume reduction surgery, and lung transplantation.
Bronchodilators
Bronchodilators are used for COPD treatment, they open up the airway tubes and allow air to more freely pass in and out of the lung tissue. There are both short-term (several hours) and long-term (12 or more hours) types of bronchodilators.
Examples of short-term bronchodilators
- albuterol.
- metaproterenol.
- levalbuterol.
- pirbuterol.
Examples of long-term bronchodilators
- salmeterol
- formoterol
- arformoterol
- indacaterol.
Anticholinergic bronchodilators
- ipratropium
- tiotropium
- aclidinium.
Other bronchodilators such as theophylline are occasionally used but are not favored because of unwanted side effects including anxiety, tremors, seizures, and arrhythmias.
Also on the market are combined drugs using steroids and long-acting bronchodilators. Roflumilast inhibits the enzyme phosphodiesterase type 4 and has been utilized in patients with symptoms of chronic bronchitis.
Stage III – short-acting bronchodilator as needed long-acting bronchodilators for cardiopulmonary rehabilitation and inhaled glucocorticoids for repeated exacerbations
Stage IV – as needed, long-acting bronchodilators, cardiopulmonary rehabilitation, inhaled glucocorticoids, long-term oxygen therapy, possible lung volume reduction surgery, and possible lung transplantation (in allopathy, stage IV has been termed “end-stage” chronic obstructive pulmonary disease)
Surgery to treat COPD?
There are three types of surgery generally available to treat certain types of patients with COPD which include
- Bullectomy surgery is the removal of giant bullae. Air-filled spaces usually located in the lung periphery that occupy lung space most often in people with emphysema are termed bullae. Giant bullae may occupy over 33% of the lung tissue, compress adjacent lung tissue, and reduce blood flow and ventilation to healthy tissue. Surgical removal can allow compressed lung tissue that is still functional to expand.
- Lung volume reduction surgery is the removal of lung tissue that has been most damaged by tobacco smoking, usually the 20% to 30% of lung tissue located in the upper part of each lung. This procedure is not done often; it is usually done on people who have severe emphysema and marked hyperinflation of the airways and air spaces.
- Lung transplantation is surgical therapy for people with advanced lung disease. People with COPD are the largest single category of people who undergo lung transplantation. In general, these people with COPD usually are at COPD stage three or four with severe symptoms and generally, without transplantation, have a life expectancy of about two years or less.
Prognosis and life expectancy of COPD treated with allopathy
- For patients with mild COPD (stage I) the prognosis is very good and they may have a relatively normal life expectancy but this decreases as the severity of staging increases.
- Patients with COPD who are admitted to an ICU have an estimated death rate of about 24% and this rate can double for people over age 65.
- The average life expectancy of a COPD patient who undergoes a lung transplant is about five years.
- Patients who have COPD and continue to smoke, have a rapid decline in FEV1, develop severe hypoxemia, develop right-sided heart failure, and/or have poor ability to do daily functions usually have a poor prognosis.
Homeopathic Treatment for chronic obstructive pulmonary disease COPD
Agaricus Muscarius
Violent attacks of coughing that can be suppressed by effort of will, worse eating, pain in head while cough lasts. Spasmodic cough at night after falling asleep, with expectoration of little balls of mucus. Labored, oppressed breathing. Cough ends in a sneeze.
Pain, with sensitiveness of spine to touch; worse in dorsal region. Lumbago; worse in open air. Crick in back. Twitching of cervical muscles. Very sensitive to cool air. Violent attacks of heat in evening. Copious sweat. Burning spots.
Calcarea Carbonicum
Tickling cough troublesome at night, dry and free expectoration in morning; cough when playing piano, or by eating. Persistent, irritating cough from arsenical wall paper. Extreme dyspnea. Painless hoarseness; worse in the morning. Expectoration only during the day; thick, yellow, sour mucus. Bloody expectoration; with sour sensation in chest. Suffocating spells; tightness, burning and soreness in chest; worse going upstairs or slightest ascent, must sit down. Sharp pains in chest from before backwards. Chest very sensitive to touch, percussion, or pressure. Longing for fresh air. Scanty, salty expectoration
Ipecacuanha
Dyspnea, constant constriction in chest. Asthma. Yearly attacks of difficult shortness of breathing. Continued sneezing; coryza; wheezing cough. Cough incessant and violent, with every breath. Chest seems full of phlegm, but does not yield to coughing. Bubbling rales. Suffocative cough; child becomes stiff, and blue in the face. Whooping-cough, with nosebleed, and from mouth. Bleeding from lungs, with nausea; feeling of constriction; rattling cough. Croup. Hemoptysis from slightest exertion. Hoarseness, especially at end of a cold. Complete aphonia.
Ambra Gresia
Asthmatic breathing with eructation of gas. Nervous, spasmodic cough, with hoarseness and eructation, on waking in morning; worse in presence of people. Tickling in throat, larynx and trachea, chest oppressed, gets out of breath when coughing. Hollow, spasmodic, barking cough, coming from deep in chest. Choking when hawking up phlegm. Palpitation, with pressure in chest as from a lump lodged there, Palpitation in open air with pale face.
Kalium Bichromicum
Voice hoarse; worse, evening. Metallic, hacking cough. Profuse, yellow expectoration, very glutinous and sticky, coming out in long, stringy, and very tenacious mass. Tickling in larynx. Catarrhal laryngitis cough has a brassy sound. True membranous croup, extending to larynx and nares. Cough, with pain in sternum, extending to shoulders; worse when undressing. Pain at bifurcation of trachea on coughing; from mid-sternum to back.
Drosera Rotundfolia
Affects markedly the respiratory organs and is the principal remedy for whooping-cough. Drosera can break down resistance to tubercle. Phthisis pulmonal; vomiting of food from coughing with gastric irritation and profuse expectoration. Spasmodic, dry irritative cough, whooping cough. yellow expectoration, with bleeding from nose and mouth, laryngitis. Rough, scraping sensation deep in the faucet and soft palate.
Causticum
Hoarseness with pain in chest; aphonia. Larynx sore. Cough, with raw soreness of chest. Expectoration scanty; must be swallowed. Cough with pain in hip, especially left worse in evening; better, drinking cold water; worse, warmth of bed. Sore streak down trachea. Mucus under sternum, which he cannot quite reach. Pain in chest, with palpitation. Cannot lie down at night. Voice re-echoes. Own voice roars in ears and distresses. Difficulty of voice of singers and public speakers.
Antimuonium Tartaricum
Rattling of mucus with little expectoration with drowsiness, debility and sweat, trembling of whole body, great prostration and faintness. Hoarseness. Rattling of mucus, but hard to expectorate. Burning sensation in chest. Cough excited by eating, with pain in chest and larynx. Edema and impending paralysis of lungs.
Coldness, trembling, and chilliness. Intense heat. Copious perspiration. Cold, clammy sweat, with great faintness. Intermittent fever with lethargic condition.
All symptoms worse, in evening; from lying down at night; from warmth; in damp cold weather; from all sour things and milk. Better, from sitting erect; from eructation and expectoration.
Chamomilla
Hoarseness, hawking, rawness of larynx. Irritable, dry, tickling cough; suffocative tightness of chest, with bitter expectoration in daytime. Rattling of mucus in child’s chest.
Pulsatilla Pratensis
Capricious hoarseness; comes and goes. Dry cough in evening and at night; must sit up in bed to get relief; and loose cough in the morning, with copious mucous expectoration. Pressure upon the chest and soreness. Great soreness of epigastrium. Urine emitted with cough. Pain as from ulcer in middle of chest. Expectoration bland, thick, bitter, greenish. Short breath, anxiety, and palpitation when lying on left side. Smothering sensation on lying down.
Cina Maritima
Gagging cough in the morning. Whooping-cough. Violent recurring paroxysms, as of down in throat. Cough ends in a spasm. Cough so violent as to bring tears and sternal pains; feels as if something had been torn off. Periodic; returning spring and fall. Swallows after coughing. Gurgling from throat to stomach after coughing. Child is afraid to speak or move for fear of bringing on paroxysm of coughing. After coughing, moaning, anxious, gasps for air and turns pale.
Light chill. Much fever, associated with clean tongue. Much hunger; colicky pains; chilliness, with thirst. Cold sweat on forehead, nose, and hands.
Ammonium Carbonicum
Hoarseness. Cough every morning. Emphysema. Burning in chest. Asthenic Pneumonia. Rattling pulmonal sounds. Slimy sputum and specks of blood. Pulmonary edema.
All symptoms worse in warm, especially in morning (warm room/bed).
Sambucus Nigra
Chest oppressed with pressure in stomach, and nausea Hoarseness with tenacious mucus in larynx. Paroxysmal, suffocative cough, coming on about midnight, with crying and dyspnea. Spasmodic croup. Dry coryza. Sniffles of infants; nose dry and obstructed. Loose choking cough. When nursing child must let go of nipple, nose blocked up, cannot breathe. Child awakes suddenly, nearly suffocating, sits up, turns blue. Cannot expire. Millar’s asthma.
Dry heat while sleeping. Dreads uncovering. Profuse sweat over entire body during waking hours. Dry, deep cough precedes the fever paroxysm.
Conium Maculate
Dry hacking cough, almost continuous; worse, evening and at night, when lying down, talking or laughing, and during pregnancy. Expectoration only after long coughing.
The patient has a cough at night on lying down. They are restless at night and tend to sit up many times due to coughing spells. A tickling sensation in the throat pit may be prominently present. A few individuals may complain of an unusually dry spot in the larynx. In some cases, a headache on coughing may arise.
Hippozaeninum
Hoarseness. Pneumonia (any type). Noisy breathing; short, irregular. Cough, with dyspepsia. Excessive secretion. Suffocation imminent. Bronchitis in the aged, where suffocation from excessive secretion is imminent. Tuberculosis.
Spongia Tosta
A remedy especially marked in the symptoms of the respiratory organs, cough, croup, thyroid gland swollen. stitches and dryness in throat, burning stinging and sore throat etc. Tickling causes cough. Clears throat constantly. Laryngeal phthisis. Goiter.
Great dryness of all air-passages. Hoarseness; larynx dry, burns, constricted. Cough, dry, barking, croupy; larynx sensitive to touch. Croup; worse, during inspiration and before midnight. Respiration short, panting, difficult; feeling of a plug in larynx. Cough abates after eating or drinking, especially warm drinks. Wheezing asthmatic cough, worse cold air and lying, head low and in warm, with profuse expectoration and suffocation. Oppression and heat of chest.
Swelling and induration of glands; also exophthalmic; cervical glands swollen with tensive pain on turning head, painful on pressure; Goiter. Itching; measles.
Viola Odorata
Pneumonia. Viral pneumonia. Dry short spasmodic cough and dyspnea; worse in daytime. Oppression of chest. Pertussis, with hoarseness. Dyspnea during pregnancy. Difficult breathing, anxiety and palpitation, with hysteria.
Corallium Rubrum
whooping and spasmodic coughs, especially when the attack comes on with a very rapid cough, and the attacks follow so closely as to almost run into each other. Often preceded by sensation of smothering, followed by exhaustion. Profuse, nasal catarrh. Cough that results from PND (post nasal dripping). Hawking of profuse mucus. Throat very sensitive, especially to air.
The cough appears in quick, short attacks that follow each other in quick succession, hysterical cough. Dry, spasmodic, suffocative cough; very rapid cough, short, barking, whooping-cough. Extreme exhaustion is felt along with the cough. A vital symptom that attends the above symptoms are extremely sensitive air passages to air (inhaled air feels cold).
Millifolium
Millifolium is and antiviral medicine. Cough with bloody sputa or in any lung disease with accompanying cough. Shortness of breath, difficulty in breathing, oppression of chest. Hemoptysis after injury or following violent exertion.
Natrum Muriaticum
Cough from a tickling in the pit of stomach, accompanied by stitches in liver and spurting of urine. Stitches all over chest. Cough, with bursting pain in head. Shortness of breath. Whooping-cough with flow of tears with cough and with salty sputum.
Kali Sulph
Rattling of mucus in chest. Post-grippe cough, especially in children. Bronchial asthma, with yellow expectoration. Cough; worse in evening and in hot atmosphere. Croupy hoarseness.
Pulsatilla Nigricans
Capricious hoarseness. Dry cough in evening and at night; must sit up in bed to get relief; and loose cough in the morning, with copious mucous expectoration. Expectoration bland, thick, bitter, greenish. Short breath, anxiety, and palpitation when lying on left side
Heper Sulph
Cough troublesome when walking. Dry, hoarse cough. Cough excited whenever any part of the body gets cold or uncovered, or from eating anything cold. Croup with loose, rattling cough; worse in morning. Choking cough. Rattling, croaking cough; suffocative attacks; has to rise up and bend head backwards. Anxious, wheezing, moist breathing, asthma worse in dry cold air.
Phosphorus
Cough from tickling in throat; worse, cold air, reading, laughing, talking, from going from warm room into cold air. Sweetish taste while coughing. Hard, dry, tight, racking cough. Congestion of lungs. Burning pains, frothy or blood-stained sputum. The phlegm may be salty or sweet to taste. Strong odors may trigger a cough. Pneumonia, with oppression.
Arsenic Album
Asthma worse midnight. Burning in chest. Suffocative catarrh. Cough worse after midnight; worse lying on back. Expectoration scanty, frothy. Darting pain through upper third of right lung. Wheezing respiration. Hemoptysis with pain between shoulders; burning heat all over. Cough dry.
Throat: Swollen, oedematous, constricted, burning, unable to swallow. Diphtheritic membrane, looks dry and wrinkled.
Bryonia Alba
Soreness in larynx and trachea. Hoarseness; worse in open air. Dry, hacking cough from irritation in upper trachea. Cough, dry, at night; must sit up; worse after eating or drinking, with vomiting, with stitches in chest, and expectoration of rust-colored sputa. Frequent desire to take a long breath; must expand lungs. Difficult, quick respiration; worse every movement; caused by stitches in chest. Cough, with feeling as if chest would fly to pieces; presses his head on sternum; must support chest. Croupous and pleuro-pneumonia. Expectoration brick shade, tough, and falls like lumps of jelly. Tough mucus in trachea, loosened only with much hawking. Coming into warm room excites cough. Heaviness beneath the sternum extending towards the right shoulder. Cough worse by going into warm room.
Throat: Dryness, sticking on swallowing, scraped and constricted. Tough mucus in larynx and trachea, loosened only after much hawking; worse coming into warm room.
Sambucus Nigra
Hoarseness with tenacious mucus in larynx. Paroxysmal, suffocative cough, coming on about midnight, with crying and dyspnea. Spasmodic croup. Dry coryza. Sniffles of infants; nose dry and obstructed. Loose choking cough. When nursing child must let go of nipple, nose blocked up, cannot breathe. Child awakes suddenly, nearly suffocating, sits up, turns blue. Cannot expire. Millar’s asthma.
Mephitis Putorius
Sudden contraction of glottis, when drinking or talking. Food goes down wrong way. False croup; cannot exhale. Spasmodic and whooping-cough. Few paroxysms in day-time, but many at night; with vomiting after eating. Asthma, as if inhaling Sulphur; cough from talking; hollow, deep, with rawness, hoarseness, and pains through chest. Violent spasmodic cough; worse at night.
Senega
Hoarseness. Hurts to talk. Bursting pain in back on coughing. Catarrh of larynx. Loss of voice. Hacking cough. Thorax feels too narrow. Cough often ends in a sneeze. Rattling in chest. Chest oppressed on ascending. Bronchial catarrh, with sore chest walls; much mucus; sensation of oppression and weight of chest. Difficult raising of tough, profuse mucus, in the aged. Asthenic bronchitis of old people with chronic interstitial nephritis or chronic emphysema. Old asthmatics with congestive attacks. Exudations in Pleura. Hydrothorax. Pressure on chest as though lungs were forced back to spine. Voice unsteady, vocal cords partially paralyzed.
Throat: Catarrhal inflammation of throat and faucets, with scraping hoarseness. Burning and rawness. Sensation as if membrane had been abraded.
Sanguineria
Continual severe cough, with circumscribed redness of cheeks, with pain in chest; with coryza, then diarrhea. Coughs in old men. Expectoration tough; difficult; rust-colored; extreme dyspnea; hepatization. Breath and sputa smell badly even to patient. Pulmonary consumption, expectoration and breath exceedingly offensive. Whooping-cough. Severe cough after whooping-cough; the cough returns every time patient takes cold. Asthma: excessive dyspnea. Hydrothorax. Hemoptysis. Pneumonia.
Mercurius Sulphuricus
Throat. Heat and sensation of constriction in throat. Dryness of tongue and throat. Burning in mouth and throat. Respiratory Organs. Roughness in throat and hoarseness. Sensation of heat in larynx. Increased expectoration of mucus from larynx” and trachea. Dyspnea; in children; hydrothorax.
Cina
Gagging cough in the morning. Whooping-cough. Violent recurring paroxysms, as of down in throat. Cough ends in a spasm. Cough so violent as to bring tears and sternal pains; feels as if something had been torn off. Periodic; returning spring and fall. Swallows after coughing. Gurgling from throat to stomach after coughing. Child is afraid to speak or move for fear of bringing on paroxysm of coughing. After coughing, moaning, anxious, gasps for air and turns pale.
Sticta Pulmonaria
Oppression of lungs. Feeling of a hard mass in chest. Sudden pain through chest from sternum to spine; difficult breathing and speaking. Pulsation from sternum down to abdomen. Coryza with expectoration of dark blood brought on by every cold, damp spell.
Tickling in larynx and trachea causing cough. Clergyman’s sore throat, characterized by great dryness of mucous membranes. Hay-fever, with dryness of membranes. Cough dry day and night; can neither sleep nor lie down; dry, noisy; severe, dry, racking with splitting. Frontal headache. Cough after influenza; after measles; after whooping-cough; barking cough night and morning. Dry spasmodic – the more he coughs the more he wants to could not stop. Dry cough causing pain in upper part of sternum.
Coccus Cacti
Constant hawking from enlarged uvula; coryza, with inflamed faucets; accumulation of thick viscid mucus, which is expectorated with great difficulty. Tickling in larynx. Sensation of a crumb behind larynx, must swallow continually; brushing teeth causes cough. Faucets very sensitive. Suffocative cough; worse, first waking, with tough, white mucus, which strangles. Spasmodic morning cough. Whooping cough attacks end with vomiting of this tough mucus. Chronic bronchitis complicated with gravel; large quantities of aluminous, tenacious mucus, are expectorated. Walking against wind takes breath away.
Bromium
Whooping cough (Use persistently for about ten days). Dry cough, with hoarseness and burning pain behind sternum. Spasmodic cough, with rattling of mucus in the larynx; suffocative. Hoarseness. Croup after febrile symptoms have subsided. Difficult and painful breathing. Violent cramping of chest. Chest pains run upward. Cold sensation when inspiring. Every inspiration provokes cough. Laryngeal diphtheria, membrane begins in larynx and spreads upward. Spasmodic constriction. Asthma; difficulty in getting air into lung. Better at sea, of seafaring men when they come on land. Hypertrophy of heart from gymnastics. Fibrinous bronchitis, great dyspnea. Bronchial tubes feel filled with smoke.
Nux Vomica
Catarrhal hoarseness, with scraping in throat. Spasmodic constriction. Asthma, with fullness in stomach, morning or after eating. Cough, with sensation as if something were torn loose in chest. Shallow respiration. Oppressed breathing. Tight, dry hacking cough; at times with bloody expectoration. Cough brings on bursting headache and bruised pain in epigastric region.
Throat: Rough, scraped feeling. Tickling after waking in morning. Sensation of roughness, tightness, and tension. Pharynx constricted. Uvula swollen. Stitches into ear.
Prognosis and life expectancy of COPD treated with Homeopathy
For patients with any stage of COPD treated with Homeopathy, the prognosis is very good and patient may have a absolutely normal life expectancy in very short treatment time period that is about one to three months.
For consultation, about your disease and Treatment, Diet etc; visit our clinic.
To order medicine by courier, please send your details at WhatsApp– +92319884588
 Dr Sayyad Qaisar Ahmed (MD {Ukraine}, DHMS, Isl. Jurisprudence); Works at “senior research officer Dnepropetrovsk state medical academy Ukraine”; is a leading Homeopathic physician practicing in
Dr Sayyad Qaisar Ahmed (MD {Ukraine}, DHMS, Isl. Jurisprudence); Works at “senior research officer Dnepropetrovsk state medical academy Ukraine”; is a leading Homeopathic physician practicing in
Al-Haytham clinic Risalpur. K.P.K, Pakistan.
(0923631023, 03119884588), K.P.K, Pakistan.
www.YouTube.com/Dr Qaisar Ahmed
www.facebook.com/ahmed drqaisar
