Steroids or corticosteroids are man-made drugs that closely resemble cortisol (a hormone that our adrenal glands produce naturally). Corticosteroids are often referred to by the shortened term “steroids.” Corticosteroids are different from the male hormone-related steroid compounds that some athletes abuse.
Thank you for reading this post, don't forget to subscribe!Types of Steroids or corticosteroids
Some steroids or corticosteroid drugs include cortisone, prednisone and methylprednisolone. Prednisone is the most commonly used type of steroid to treat certain rheumatologic diseases (like rheumatoid arthritis or lupus).
How are Steroids or corticosteroids given?
Steroids or corticosteroids drugs are available in several forms that vary in how easily they dissolve or how long they stay in the body.
Steroids might be given locally, to the precise place where a problem exists, or systemically, which means throughout the “system” or body.
Examples of local steroid treatments include joint injections, eye drops, ear drops and skin creams, respiratory sprays etc. Systemic steroid treatments include oral and/or respiratory medicines or medicine that is delivered directly into a vein (intravenously or IV) or muscle (intramuscularly) or lungs. Systemic steroids circulate through the bloodstream to various body sites.
When possible, local steroid treatments are prescribed instead of systemic steroids to reduce the risk of side effects.
How do Steroids or corticosteroids work?
Steroids or corticosteroids work by decreasing inflammation and reducing the activity of the immune system. Inflammation is a process in which the body’s white blood cells and chemicals can protect against infection and foreign substances such as bacteria and viruses. In certain diseases, however, the body’s defense system (immune system) doesn’t function properly. This might cause inflammation to work against the body’s tissues and cause damage. Signs of inflammation include:
- Redness.
- Warmth.
- Swelling.
- Pain.
Steroids reduce the production of chemicals that cause inflammation. This helps keep tissue damage as low as possible. Steroids also reduce the activity of the immune system by affecting the way white blood cells work.
When advise steroids?
Steroids or corticosteroids are used to treat many conditions in which the body’s defense system doesn’t work properly and causes tissue damage. Steroids may be the main therapy for certain diseases. For other conditions, steroids might only be used sparingly or when other measures have not been successful.
Steroids are used in the treatment for certain rheumatologic or other inflammatory conditions, such as:
- Systemic vasculitis (inflammation of blood vessels).
- Asthma, Bronchitis, Pneumonia etc.
- Myositis (inflammation of muscle).
- Rheumatoid arthritis (chronic inflammatory arthritis).
- Systemic lupus erythematosus (a generalized disease caused by abnormal immune system function).
How are Steroids or corticosteroids beneficial?
When inflammation threatens to damage critical body organs, steroids can be organ-saving and in many instances, life-saving. For example, steroids may prevent the worsening of kidney inflammation, which could lead to kidney failure in people who have lupus or vasculitis and/or Pneumonia, COVID, SARC etc.
Low doses of steroids might provide significant relief from pain and stiffness for people with rheumatoid arthritis, respiratory diseases etc. Short-term use of higher doses of steroids might help a person recover from a severe flare-up of arthritis and/or other infection and/or inflammation.
How will a doctor decide if steroids are the right treatment?
The decision to prescribe steroids is always made on an individual basis. A doctor provider will consider patient’s age, physical activity, and other medicines he/she is taking. The doctor will also make sure patient understand the potential benefits and risks of steroids side effects before patient start taking them.
The potential benefits and risks of steroids vary with:
- The nature and severity of the disease being treated.
- The presence or absence of other treatment alternatives.
- The presence or absence of other significant medical problems.
Side effects of Steroids or corticosteroids
The side effects of Steroids or corticosteroids depends on the dose, type of steroid and length of treatment. Some side effects are more serious than others. Common side effects of systemic steroids include:
- Increased or decreased appetite (liver malfunctioning).
- Weight gain.
- Changes in mood.
- Muscle weakness.
- Blurred vision.
- Increased growth of body hair.
- Easy bruising.
- Lower resistance to infection.
- Swollen, “puffy” face (due to liver and/or kidneys malfunctioning).
- Acne.
- Osteoporosis (bone weakening disease).
- Onset of, or worsening of diabetes.
- Onset of, or worsening of, high blood pressure.
- Stomach irritation.
- Nervousness, restlessness.
- Difficulty sleeping.
- Cataracts or glaucoma.
- Water retention, swelling, edema.
Infection
Long-term steroids can suppress the protective role of immune system and increase the risk of infection.
Self-care-tips:
- Since steroids can decrease immunity to infection, patient should have a yearly flu shot as long as patient is on steroids. If patient is on steroids for a prolonged period of time, he/she should also discuss with his/her doctor the possibility of getting “Pneumovax,” (vaccination against a certain type of pneumonia) as well as “Prevnar 13,” another pneumonia vaccine. Shingles vaccination may also be considered.
- Signs of possible infection, such as high fever, productive cough, micturition (pain while passing urine), or large “boils” on the skin should have prompt medical attention.
Gastrointestinal symptoms
Steroids or corticosteroids increase the risk of developing ulcers and gastrointestinal bleeding, especially if patient take these medications along with non-steroidal anti-inflammatory drugs (NSAIDs). If at all possible, don’t combine steroids with NSAIDs. If patient is on low-dose aspirin, physician may want to continue this when patient take the prednisone, but might consider adding a medication for gastrointestinal and renal protection during the course of steroids.
Self-care tips:
- Patient have to report to the physician any severe, persistent abdominal pain or black, tarry stools.
- Advise steroid mediation after a full meal or with antacids, as this may help reduce irritation of the stomach. Steroids can increase or decrease appetite due to its side effects on gastrointestinal tract especially on liver.
Can Steroids or corticosteroids use cause osteoporosis?
Steroids or corticosteroids therapy can cause thinning of the bones (osteopenia and osteoporosis), and increase the risk of bone fractures. At the beginning or before steroid therapy, many patients will be asked to have a bone density test, especially if the steroid dose is high. If density is low, the bone density study It will be repeated in the future to assess the effectiveness of measures the patient will be using to prevent bone loss. Preventative strategies are important: a patient can lose 15% to 30% bone mass within the first six months of corticosteroid therapy.
Self-care tips:
- Most people taking corticosteroids will need to take a calcium supplement unless they can get enough calcium from their diet.
- The minimal daily requirement of vitamin D is 800 international units (UI) daily, and most people on corticosteroids should take this amount. Physician may check patient’s vitamin D level and see if patient actually need a higher dose.
- Smoking and alcohol increase the risk of osteoporosis, so stop or limiting these will be helpful.
- Weight-bearing exercise is helpful in stabilizing bone mass.
- People on corticosteroids who have low bone density may be put on vit-D and calcium supplements.
- Assess risk of falls. patient should make a thorough examination of her/his home and correct situations that might result in a fall, such as eliminating scatter rugs and any obstacles between bedroom and bathroom, and installing night lights.
Can Steroids or corticosteroids make patients gain weight?
Steroids or corticosteroids affect liver function, metabolism and how one’s body deposits fat. This can increase appetite, leading to weight gain, and in particular lead to extra deposits of fat in the abdomen.
Insomnia
Steroids may impair one’s ability to fall asleep, especially when they are taken in the evening.
Self-care tips:
- If possible, the physician will try to have you take your entire daily dose in the morning. This may help you sleep better at night.
Mood changes
Steroids, especially in doses over 30 milligrams per day, can affect patient’s mood. Some people can feel depressed, some extremely “up” without any apparent reason. Just being aware that steroids can do this sometimes makes it less of a problem. When the steroids are absolutely necessary, sometimes another medication can be added to help with the mood problem (which means some newer side effects of that new drug).
Fluid retention and elevated blood pressure
Because cortisone is involved in regulating the body’s balance of water, sodium, and other electrolytes, using these drugs can promote fluid retention and sometimes cause or worsen high blood pressure.
Self-care tips:
- Patient should watch for swelling of her/his ankles, and report this to the doctor. Occasional patients benefit from diuretics (only in case if patient has no any renal disease/complications). Low sodium diet helps reduce fluid accumulation and may help control blood pressure, but low sodium diet severely effects on liver function, cardiac function (irregular heart beats), decreases bone density, effects on eyesight and brain function and minimise cell’s lifespan.
- Have your blood pressure monitored regularly while you are on steroids, especially if you have a history of high blood pressure. Steroids can raise blood pressure.
Elevated blood sugar
Since cortisone is involved in maintaining normal levels of glucose (sugar) in the blood, long-term use may lead to elevated blood sugar or even diabetes.
Self-care tips:
- Your blood sugar should be followed while you are on steroids, especially if you are a diabetic, because corticosteroids can raise blood sugar.
Eye problems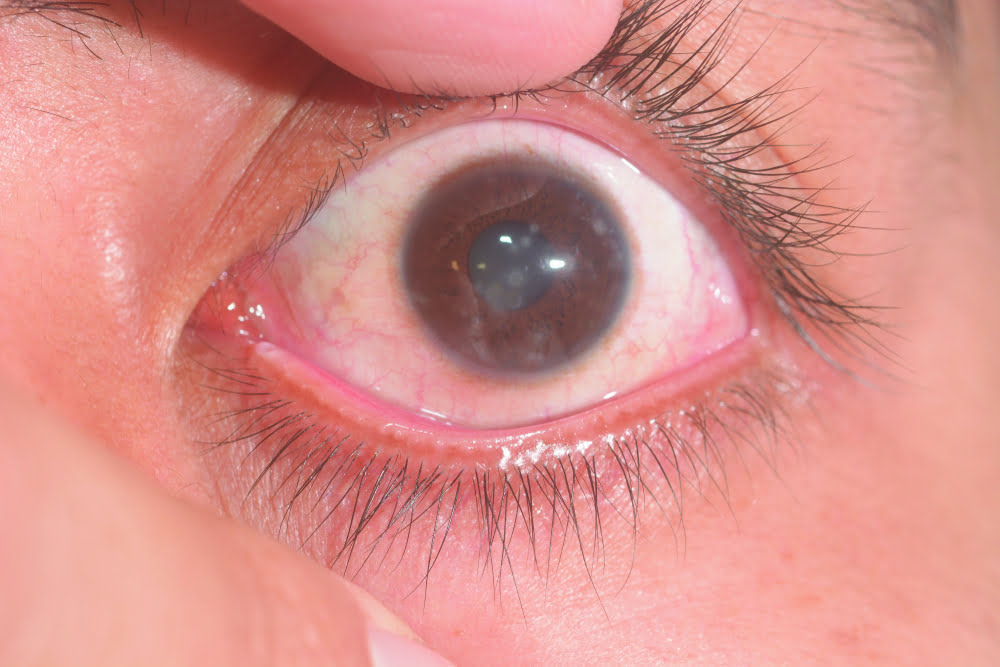
Steroids or corticosteroids can cause cataracts or glaucoma (increased pressure in the eye).
Self-care tips:
- If you have a history of glaucoma or cataract follow up closely with the ophthalmologist while on steroids. If you develop any visual problems while on steroids, you will need to see the ophthalmologist. Blurred vision after starting corticosteroids is a serious problem.
Atherosclerosis (hardening of the arteries)
It is confirmed that Steroids or corticosteroids increases the rate of “hardening of the arteries,” which increases the heart, renal and brain disease (failure and/or strokes) rates in healthy people.
Self-care tips:
- Recent studies shows (year 2022) that low or high cholesterol diet have no any good or bad effects on overall health especially heart and arteries. But if you develop signs suggesting heart problem after starting corticosteroids, such as chest pain, get medical attention quickly. Work with your physician to address any heart and/or arterial risks that can be modified.
Aseptic necrosis
- Steroids or corticosteroids, particularly at higher doses for long periods of time, can lead to damage to bones, called aseptic necrosis (also known as osteonecrosis or avascular necrosis). This can happen in a number of joints, but the hip is the most common.
Self-care tips:
- Hip pain, especially if you have no known hip arthritis, could be an early sign of this damage. Report this to your doctor.
How can the side effects of steroids be minimized?
To minimize the side effects of steroids, healthcare providers follow several guidelines:
- Use steroids only when necessary.
- Watch the patient closely to detect early signs of serious side effects.
- If possible, use local steroids for local problems or advise Homeopathic medicines.
- Use the smallest dose needed to control the disease.
- Reduce the dose gradually as long as the disease remains under control.
- Monitor blood pressure and blood sugar often.
- Monitor bone density and prescribe drugs and supplements to help bone health.
There are other ways to prevent certain side effects, and these need to be discussed individually with your healthcare provider to start Homeopathic treatment instead.
Steroids or corticosteroids withdrawal syndrome
When anti-inflammatory steroids have been taken for some time and then are rapidly withdrawn, our adrenal gland (which makes our body’s steroid hormones) can be sluggish in making our own steroid hormone. Taking anti-inflammatory steroids can lead to inhibition of the complex pathway that leads to our body’s production of anti-inflammatory steroid hormone (cortisol). Taking these anti-inflammatory steroids can suppress the hypothalamus, as well as the pituitary gland, which are all involved the process of stimulating the adrenal gland to make cortisol.
For example, the pituitary gland production of ACTH (which stimulate the adrenal to make cortisol) can be inhibited. The adrenal gland itself can also show some suppression of its ability to make cortisol.
Rapid withdrawal of steroids may cause a syndrome that could include fatigue, joint pain, muscle stiffness, muscle tenderness, fever etc. These symptoms could be hard to separate from those of the underlying disease. Even with slower withdrawal of steroids, these symptoms are possible.
At times, rapid withdrawal of steroids can lead to a more severe syndrome of adrenal insufficiency. This can cause symptoms and health problems such as drops in blood pressure, as well as chemical changes in the blood such as high potassium or low sodium. Sometimes this can be set off by injuries or a surgical procedure. Because of this, make sure the doctors always know if patient have been treated with steroids in the past, especially in the past year, so the doctor can be on the alert for the development of adrenal, liver and/or renal insufficiency at times such as a surgical procedure.
In Homeopathic medicines there are lots of medicines to avoid any allopathic steroid/corticosteroid and treat patient more securely in less time and for life time.
P. S : This article is only for doctors having good knowledge about Homeopathy and allopathy, for learning purpose(s).
For proper consultation and treatment, please visit our clinic.
Location, address and contact numbers are given below.
NoN of above mentioned medicine(s) is/are not the full/complete treatment, but just hints for treatment; every patient has his own constitutional medicine along with these mentioned above.
To order medicine by courier, please send your details at WhatsApp– +923119884588
 Dr. Sayyad Qaisar Ahmed (MD {Ukraine}, DHMS), Abdominal Surgeries, Oncological surgeries, Gastroenterologist, Specialist Homeopathic Medicines.
Dr. Sayyad Qaisar Ahmed (MD {Ukraine}, DHMS), Abdominal Surgeries, Oncological surgeries, Gastroenterologist, Specialist Homeopathic Medicines.
Senior research officer at Dnepropetrovsk state medical academy Ukraine.
Location: Al-Haytham clinic, Umer Farooq Chowk Risalpur Sadder (0923631023, 03119884588), K.P.K, Pakistan.
Find more about Dr Sayed Qaisar Ahmed at :
https://www.youtube.com/Dr Qaisar Ahmed
